July 9, 2025
Canada abolishes disabilities minister as assisted dying expansion continues

July 4, 2025
Assisted suicide described as “an alternative to decent care” after Canadian man’s death after neglect

July 3, 2025
Hospice boss warns patients may feel forced to choose fully funded assisted suicide over cash-strapped…

July 2, 2025
Councillor who would have chosen assisted suicide in 'moment of despair' speaks out against Leadbeater…

July 1, 2025
Lord Falconer says Lords shouldn't block assisted suicide Bill backed by Commons – despite him…

June 30, 2025
Assisted suicide Bill "would put a price on my head", says peer with a disability

June 27, 2025
Canadian veteran seeking help for PTSD offered euthanasia

June 24, 2025
Reform UK expected to pledge to repeal proposed assisted suicide and abortion to birth laws…
June 23, 2025
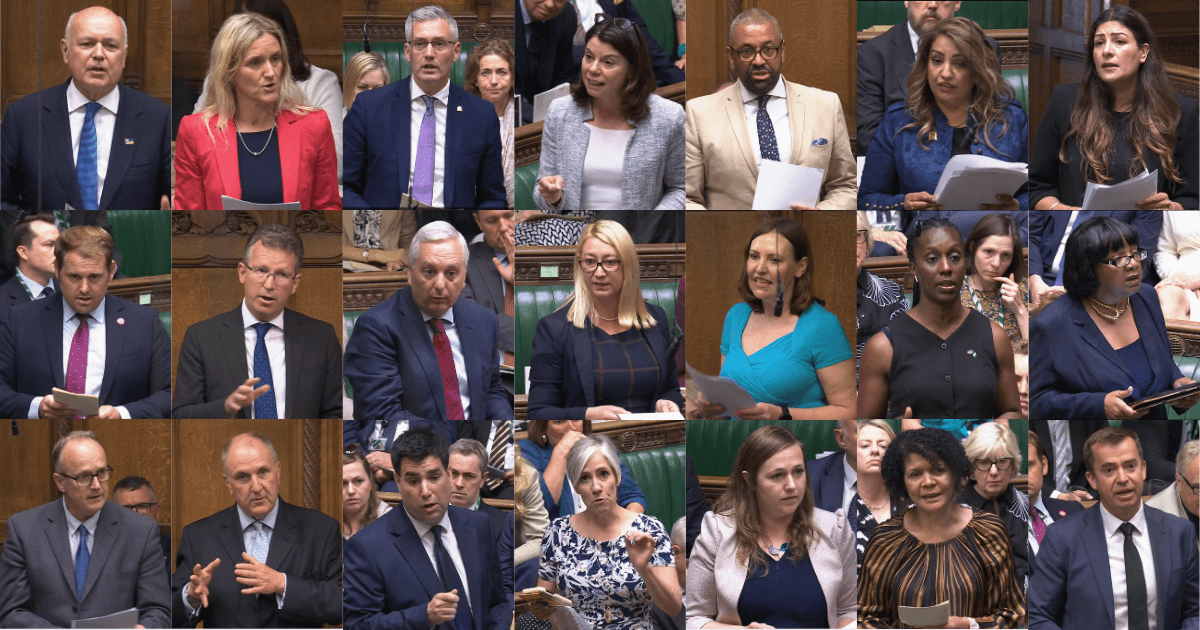
Third Reading wrap-up: MPs vote through assisted suicide Bill in narrowest margin yet, as opposition…

June 11, 2025
Royal College of Pathologists voices concerns over assisted dying Bill

June 10, 2025
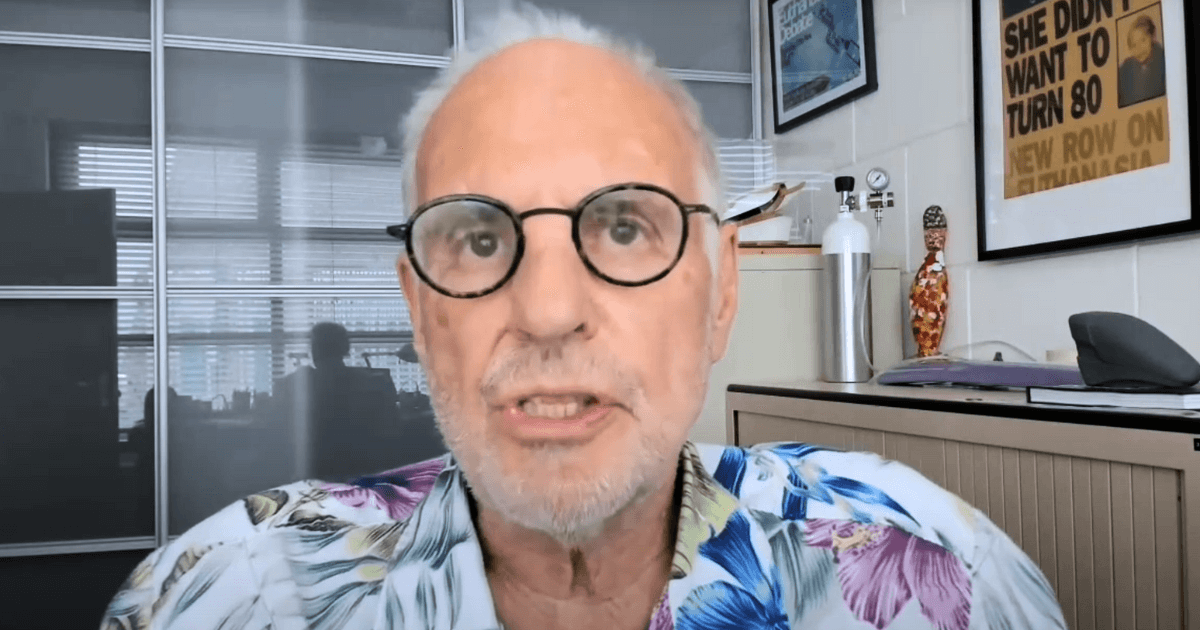
Leadbeater refuses to back amendment to ban ‘Dr Death’s suicide pods

June 6, 2025
More MPs change their mind to indicate they will vote against assisted suicide Bill

June 4, 2025
Man nearly dies after allegedly taking partner's assisted suicide drugs
June 2, 2025
‘Dr Death’ proposes implant to kill dementia patients who miss daily prompts

May 28, 2025
Justice Secretary condemns inadequate process of assisted suicide Bill

May 19, 2025
Royal College of Physicians warn of “deficiencies” in assisted suicide Bill