Marie Stopes International

50% increase in abortions in first two weeks of year according to abortion provider

Senior civil servant spiked woman’s orange juice with abortion drug so she would lose baby,…

54 years of abortion: 9,900,961 lives lost since 1967 — one unborn baby every 2.5…

Leading international abortion provider admits 1 in 20 women have fragments of baby/placenta left inside…

5th Marie Stopes Australia abortion clinic closes due to financial difficulties

Marie Stopes Australia closes 4 abortion clinics

International Planned Parenthood plan to sue UK Govt for cuts to abortion funding
![Marie Stopes International’s first abortion clinic closes 8 MSI Reproductive Choices (formerly known as Marie Stopes International) permanently closed its flagship central London clinic last Friday. The clinic performed 4,235 abortions over 2018 and 2019. The Marie Stopes House clinic, located on Whitfield Street in Bloomsbury, was Britain's first family planning clinic. It moved from its initial location in Holloway, North London in 1925. After Stopes’s death in 1958, the clinics continued to operate, however by 1975 the Marie Stopes Foundation was bankrupt and in 1976 the clinic was taken over by Tim Black and Phil Harvey. They purchased the lease on the Whitfield Street clinic and re-founded the organisation as ‘Marie Stopes International’. Black and Harvey also co-founded global abortion provider Population Services International (PSI) together in 1970. In the same year, they co-founded ‘Adam and Eve’, now one of the largest pornography companies in the world, which has given more than £7.5 million to MSI Reproductive Choices. Harvey is also the founder and former president of global abortion provider DKT International. In 2017, DKT acquired the worldwide rights to distribute the Ipas manual vacuum aspiration (MVA) technology, which it now markets and distributes in over 100 countries around the world. Vacuum aspiration is the procedure that uses a vacuum source to remove an embryo or fetus through the cervix. A history of racism and eugenics It was only in November 2020 that Marie Stopes International was renamed "MSI Reproductive Choices" due to Stopes’ well-documented views on eugenics, despite the company claiming that “The name of the organisation has been a topic of discussion for many years”. In the wake of this change, the organisation was ridiculed due to its new name’s resemblance to the Movimento Sociale Italiano (MSI), the Italian Social Movement. The party was formed in 1946 by supporters of the former Italian dictator, Benito Mussolini. MSI is regarded as a successor of Mussolini’s Republican Fascist Party (PFR). Marie Stopes publicly advocated for the involuntary sterilisation of several groups she deemed unfit for parenthood, including people with disabilities, addicts, ‘subversives’, criminals, and those of mixed ethnic origin. Stopes even wrote her own son out of her will because he married a woman who had bad eyesight. In her writings, Stopes called for laws that allowed the forced sterilisation of what she described as the “hopelessly rotten and racially diseased” and wrote fiercely against interracial marriage. She also corresponded with Adolf Hitler, and in August 1939 enclosed a book of her love poems to him. Profits prioritised over patients In 2017, a damning report from the UK’s Care Quality Commission (CQC) accused Marie Stopes International (now MSI Reproductive Choices) of paying staff bonuses for persuading women to have abortions. At all 70 Marie Stopes clinics, inspectors from the Care Quality Commission found evidence of a policy that saw staff utilise a high-pressure sales tactic, calling women who had decided against having an abortion to offer them another appointment. Another report in 2017 showed that nearly 400 botched abortions were carried out in two months at Marie Stopes clinics. The report also outlined that in another three-month period, 11 women needed emergency transfers to hospital after difficulties at facilities run by the abortion provider. In 2016, Marie Stopes International was forced to suspend abortion services for a month after an unannounced inspection by the CQC found 2,600 safety flaws at Marie Stopes International abortion clinics in the UK including doctors going home and leaving women under sedation to be supervised by nurses and healthcare assistants, fetuses being put in waste bins rather than cremated and staff trying to give a vulnerable, visibly distressed woman an abortion without her consent. The inspectors also found that almost half of nurses working at the clinics had not been trained to do resuscitation, safety incidents including medical blunders and equipment failures had increased by a third in a year and doctors were signing off up to 60 consent forms at a time when they were meant to be making a thorough assessment. One doctor filled in up to 26 consent forms in two minutes. Eleven years of peaceful pro-life demonstrations The area surrounding the Whitfield Street Clinic has been a large focus of peaceful pro-life activism since 2010 when a regular vigil was launched. The Good Counsel Network, who worked with 40 Days for Life to organise these events, wrote in a blog post: “In recent years some Marie Stopes Staff [from the Whitfield St Clinic] have come to us seeking help to find alternative jobs. They told us they thought the job with MS would involve helping vulnerable pregnant women who were aborting because of difficult situations but found that they were often facing abusive clients with aggressive partners, and that there was a big focus on money rather than on client health or staff wellbeing”. They also detailed how, “During one of several 40 Days at Whitfield Street, Marie Stopes were doing internal building work. The builders often arrived very early, so Marie Stopes staff started leaving the clinic front door key in the flowerpot on the doorstep for the builders to let themselves in”. “It became a running joke between ourselves and the builders that the key was being left. And yet no pro-lifer ever interfered in any way with the abortion centre”. MSI Reproductive Choices has recently opened two new clinics in Hammersmith and Camden. Spokesperson for Right To Life UK, Catherine Robinson, said: “All the data indicates that the abortion numbers for 2020 are likely to be the highest ever recorded in the UK. MSI clearly has not let this ‘opportunity’ go to waste after opening two new London clinics”. “However, the closing of the historic Whitfield Street clinic, which Stopes herself moved her original clinic to in 1925, is of course welcomed by pro-lifers, many of whom who have selflessly spent over a decade peacefully demonstrating there, and who have provided invaluable help to pregnant women and MSI staff seeking a better future”.](https://righttolife.org.uk/wp-content/uploads/2021/06/marie-stopes-clinic-closes.jpg)
Marie Stopes International’s first abortion clinic closes

Four new abortion clinics to open in South East England

Abortion giant adopts 20th century fascist party’s name in embarrassing rebrand
Abortion provider Marie Stopes International change name to hide links with eugenics

Marie Stopes International hoping to recruit more students into 'abortion care'

Record £308m income for Marie Stopes, with UK taxpayer being single biggest donor
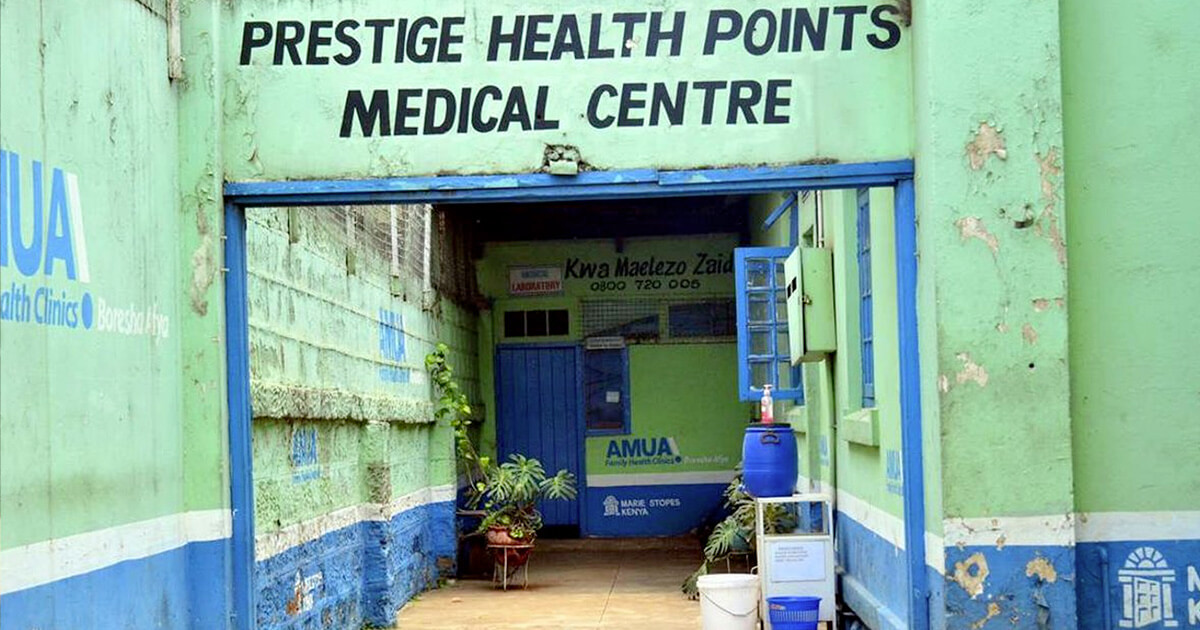
Marie Stopes franchise forced to close after 'fake' doctors found performing illegal abortions

Censorship zone in Manchester will deny pregnant women emotional and practical support

