Strong opposition from MPs has resulted in the Government rejecting calls for a review on assisted suicide despite the best efforts from large pressure groups in favour of assisted suicide.
This follows the news that an attempt to introduce assisted suicide to the Isle of Man has failed.
MPs received thousands of emails from constituents ahead of the debate urging them to attend and speak in opposition to the assisted suicide lobby’s campaign.
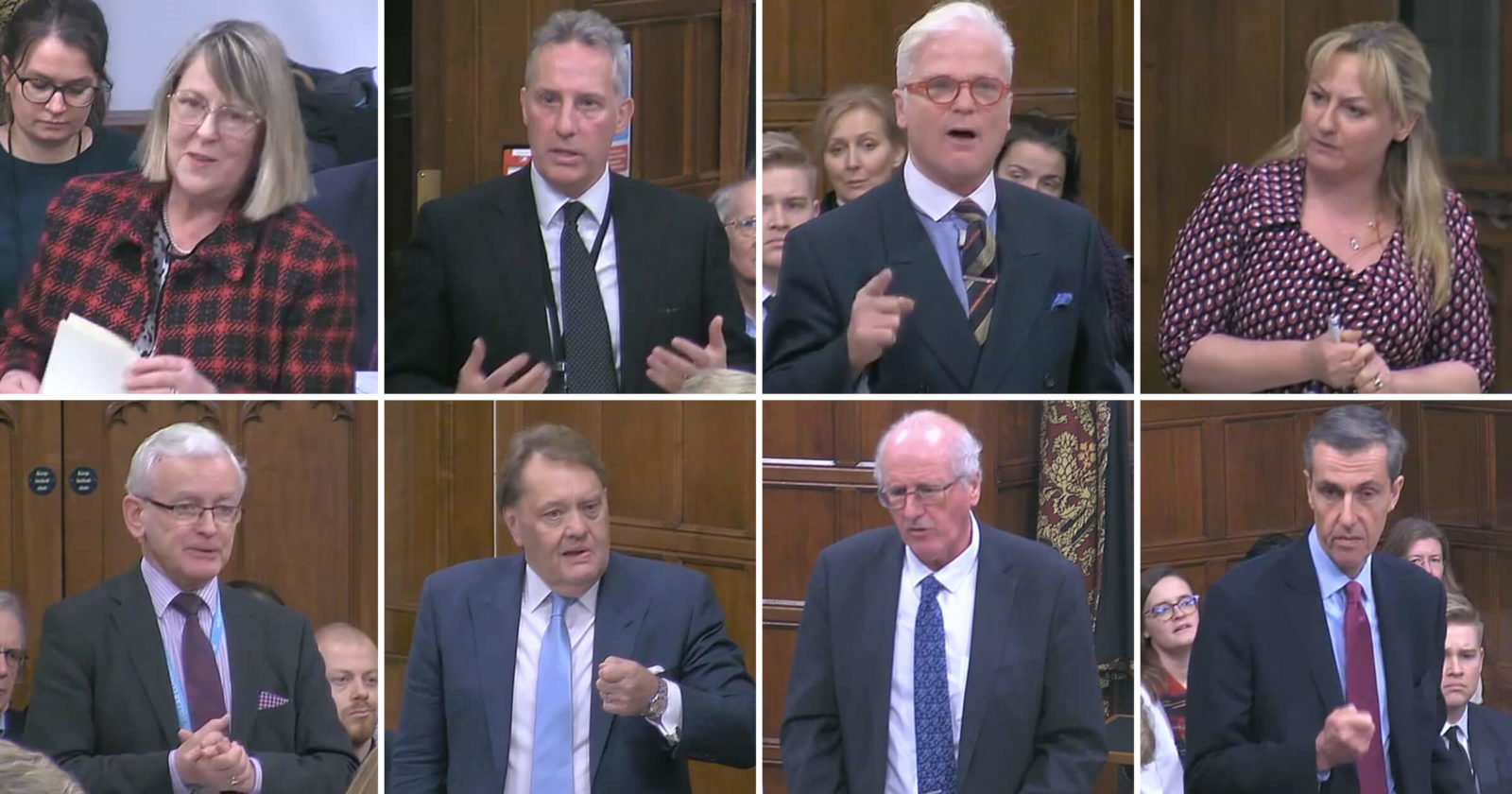
A large turnout of MPs, including Sir Desmond Swayne, Sir John Hayes, Fiona Bruce, Dr Lisa Cameron, Andrew Selous and Martin Vickers spoke strongly against assisted suicide in the debate.
Fiona Bruce, Chair of the All-Party Parliamentary Pro-Life Group, said disability groups are “extremely concerned” about what has happened in other countries that have introduced assisted suicide legislation.
She noted that in the US State of Oregon the majority of those applying for assisted suicide now cite “fear of being a burden” as their major end-of-life concern. Adding that “far fewer cite pain concerns.”
In Canada, “under the 2016 law that has allowed terminally ill people to request assisted suicide and euthanasia, safeguards have been ignored, removed and extended to non-terminally ill people such as those with depression.”
“In July a depressed but otherwise healthy man was killed by lethal injection, despite not being terminally ill. Another man who suffers from a neurological disease actually recorded hospital staff offering him a medically assisted death, despite repeated statements that he did not want to die.
“Only this week, on Tuesday, there was an article in The Times about three Belgian doctors on trial in relation to the euthanasia of someone reported to have a personality disorder and autism. The family believes that she was depressed but that she did not, as required by Belgian law, have a serious and incurable disorder.”
In these cases, she said: “The point to note is that, regardless of the wording of eligibility criteria in legislation, in practice safeguards are often discarded, and vulnerable and depressed people are assisted to end their lives.”
“Rather than assisting vulnerable people to commit suicide, or administering euthanasia, we should be looking to improve palliative care provision and mental health treatment… Marie Curie estimates that 25% of cancer patients do not currently get the palliative care that they need.”
Rounding off her speech, she exclaimed: “The UK is a pioneer in palliative medicine and a world leader in palliative care. Let us keep it that way!”
A large number of MPs mirrored Fiona’s call for improved mental-health and palliative care, over the introduction of an extreme assisted suicide law, in a renewed effort to assist people to live.
Dr Lisa Cameron, Chair of the All-Party Parliamentary Group for Disability, said: “Often, when people face debilitating illness or very difficult life events, suicide may come to their minds. Does she agree that at such times, we should provide better mental health support, psychological support and counselling to enable people to come to terms with their feelings and look much more positively towards their abilities and the contribution they make?”
Expressing his concerns about a potential review into the law on assisted suicide, Jim Shannon argued: “The answer is not legalising assisted suicide. The answer is to help, to support and to be compassionate towards families. Does she acknowledge the good work that is done by many charities, particularly Macmillan, whose compassion and love make the unimaginable a little bit more bearable?”
His fellow DUP colleague, Ian Paisley, continued this point by saying: “We should be asking the positive, strong question: how much palliative care and support can we give people at the greatest point of need?”
He added: “We parliamentarians should be prepared to offer hope to people, not to say, as others have said, ‘You’re now a burden. It’s time to shuffle off this mortal coil.’”
Baroness Finlay has introduced an Access to Palliative Care and Treatment of Children Bill to the House of Lords. This bill aims to highlight the necessity of speciality training for palliative care; to ensure that children, babies, and those with learning disabilities receive palliative care; and, the responsibility of Clinical Commissioning Groups to identify, fund support and provide services to those with palliative care needs.
Other concerns raised by MPs included the change it would bring in the relationship between a doctor and a patient.
Martin Vickers MP said the relationship between a doctor and patient is one the UK should treasure. “Rather than opening the door to assisting us to die, patients—all of us—need to have confidence that our medical professionals are striving to keep us in good health and alive,” he added.
Extending this point, Sir Desmond Swayne MP noted the large number of assisted suicide deaths in the Netherlands and asked wether we are prepared to “fundamentally change the nature of the medical profession, when the clinician who brings healing is also the clinician who brings death?”
Another argument made by MPs was the valuation of life, and how legalising assisted suicide would fundamentally change how we value life as a society. Making this point was Sir John Hayes MP who said: “Although life, as I have described it, is momentary, each moment is precious. The life of profoundly disabled people is precious, and the life of those weak, wizened, sick and infirm people is precious.”
Highlighting how the valuation of life would change, Andrew Selous MP said: “We need to be very careful to ensure that old and sick people do not feel a pressure to end their lives, perhaps from their children, who might want to inherit their assets and to whom they may feel they are being a burden.”
Not a single doctors group or major disability rights organisation in the UK supports changing the law, including the British Medical Association, the Royal College of General Practitioners, the Royal College of Physicians, the British Geriatric Society and the Association for Palliative Medicine.
Parliament has consistently rejected attempts by the assisted suicide lobby to introduce assisted suicide, with 330 to 118 voting against introducing assisted suicide in 2015.
Assisted suicide pressure groups cite a poll that shows there is widespread support for legislation of assisted suicide, yet experts have heavily criticised the polling as deeply flawed. In fact, when asked questions that drill down into the merits of the debate, the percentage of those in support drops dramatically.